Unlocking New Treatment Insights for Children With Epileptic Spasms: The TOPAMAD Trial
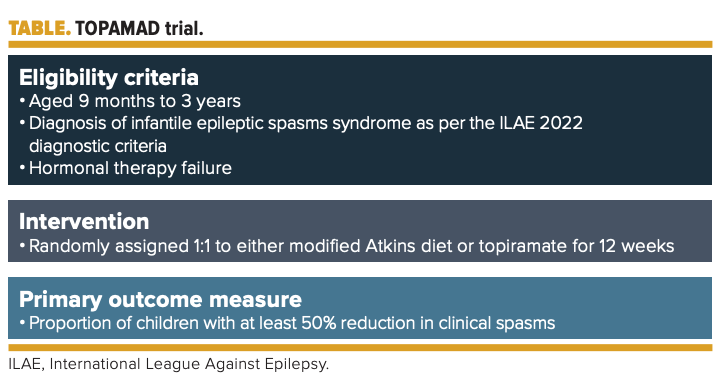
TOPAMAD will include 70 children with epileptic spasms who experienced hormonal therapy failure to determine whether modified Atkins diet or topiramate is a more effective treatment approach.
EPILEPTIC SPASMS, a specific type of seizure seen in an epilepsy syndrome of infancy and childhood, has been typically managed through hormonal therapy such as adrenocorticotropic hormone (ACTH); prednisolone; or vigabatrin, an antiseizure medication (ASM). Also referred to as West syndrome, these types of seizures typically begin between the ages of 4 and 8 months and stop by around the age of 4 or 5 years. Some children will develop other types of seizures, such as Lennox-Gastaut syndrome (LGS), which is a rare epileptic disorder of later childhood.
Suvasini Sharma, MD

Despite a handful of therapeutic options, some children with epileptic spasms remain drug resistant to treatment. The TOPAMAD trial (NCT05958160), a randomized, open-label study, will compare the efficacy and tolerability of topiramate, a commonly used second-line agent, with modified Atkins diet in children with epileptic spasms refractory to hormonal treatment.1
The results of the study, led by Suvasini Sharma, MD, an associate professor at the Lady Hardinge Medical College in New Delhi, India, are intended to guide clinicians to the best treatment options for this patient population. The study expects to enroll 70 participants aged 9 months to 3 years who have a diagnosis of infantile epileptic spasms per the International League Against Epilepsy 2022 diagnostic criteria and have experienced hormonal therapy failure with either oral prednisolone or ACTH. The study’s primary outcome evaluates the proportion of children with at least a 50% reduction in clinical spasms over a 12-week treatment period.
Secondary outcomes of the study include the proportion of patients with clinical spasm cessation; improvements of at least 1 point in Burden of Amplitudes and Epileptiform Discharges score; and adverse events (AEs), or safety, in each group. Both the modified Atkins diet (considered the experiment) and topiramate will be added to the ongoing ASM regimen.
The modified Atkins diet is a change to the traditional ketogenic diet to make it less restrictive. Along with the medium chain triglyceride diet and low glycemic index treatment, it is 1 of 3 alternative diets used to treat patients with epilepsy. Some of its specific differences from ketogenic diets are that there is no fluid or calorie restriction, there are no restrictions on proteins, and foods are not weighed or measured; however, carbohydrate counts are monitored by patients and/or parents.2
Research on the modified Atkins diet has expanded significantly over the years, including some studies in infantile spasms. A 2021 study (NCT03807141) of children (n = 91) aged 9 months to 3 years who had experienced hormonal therapy failure continued to support the diet’s efficacy and safety in this patient population. That study, also led by Sharma, randomly assigned children to modified Atkins diet either immediately or after a delay of 4 weeks.3
At the end of the 4-week treatment period, 11 children in the diet group were spasm free compared with none in the control group (P ≤ .001). Thirty (65.2%) participants in the diet group had at least a 50% reduction in spasms compared with none in the control group. The median time to achieve spasm cessation was 10 days (IQR, 9-20), and 9 of these participants had resolution of hypsarrhythmia on electroencephalography.
Topiramate, the comparator drug, has multiple mechanisms of action, including the state-dependent inhibition of sodium channels, the potentiation of γ-aminobutyric acid–induced chloride influx, the blockade of glutamate-related excitatory neurotransmission, and the inhibition of carbonic anhydrase. It has been used as a monotherapy and adjunctive treatment of partial-onset and generalized tonic-clonic seizures in adults, as well as for partial seizures in children. Additionally, it has been shown to be effective when used as adjunctive therapy for the management of LGS.
The literature on topiramate in infantile spasms is limited, with few studies since it became marketed. A 2006 trial included 20 patients who received an initial dose of 1 mg/kg/d, with a progressive titration of 1 mg/kg/week until their spasms were controlled, and a maximum dose of 12 mg/kg/day was achieved. Results showed that 30% of the patients became spasm free during the study and 70% had at least a 50% reduction in seizure frequency. This study differed from TOPAMAD in that it assessed effectiveness and tolerability of topiramate when used as the initial treatment rather than in the second line for patients with newly diagnosed infantile spasm.4
Topiramate, sold in both tablet and capsule forms, can be taken with or without food. Some of the common AEs while on the therapy include fatigue, confusion, dizziness, depression, and difficulty with memory.
REFERENCES
1. Modified Atkins diet versus topiramate in children with epileptic spasms refractory to hormonal treatment: a randomized open-label study (TOPAMAD). Clinicaltrials.gov. Updated July 24, 2023. Accessed February 5, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT05958160
2. Modified Atkins diet. Epilepsy Foundation. Updated February 4, 2022. Accessed February 5, 2024. https://www.epilepsy.com/treatment/dietary-therapies/modified-atkins-diet
3. Sharma S, Goel S, Kapoor D, et al. Evaluation of the Modified Atkins diet for the treatment of epileptic spasms refractory to hormonal therapy: a randomized controlled trial. J Child Neurol.2021;36(8):686-691. doi:10.1177/08830738211004747
4. Kwon YS, Jun YH, Hong YJ, Son BK. Topiramate monotherapy in infantile spasm. Yonsei Med J.2006;47(4):498-504. doi:10.3349/ymj.2006.47.4.498